Bishop Score Calculator
The Bishop Score (also known as the Pelvic Score) is the most widely used method for estimating cervical favorability for induction of labor. Points are assigned to five cervical exam components: dilation, effacement, station, cervical consistency, and position. The calculator below automatically computes a total Bishop score.
If the Bishop score is 8 or greater, the chances of having a vaginal delivery are good and the cervix is said to be favorable or "ripe" for induction. If the Bishop score is 6 or less, the chances of having a vaginal delivery are low and the cervix is said to be unfavorable or "unripe" for induction.
A simplified Bishop score using only dilation, station, and effacement may be as predictive of successful induction as the original full Bishop score. A simplified Bishop score of 5 had a similar predictive value for successful vaginal delivery as an original Bishop score greater than 8.
How the Points Are Assigned
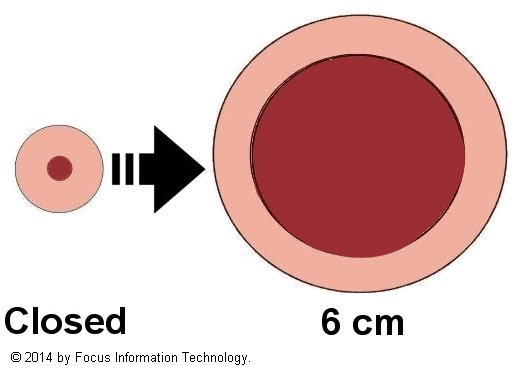
Dilatation (Dilation)
Dilation refers to how open the cervix is, measured in centimeters. A penny is approximately 2 cm across and can be used as a visual reference. Points range from 0 (closed cervix) up to 3 for a cervix dilated to 5–6 cm or greater.

Effacement
Effacement (also called shortening or thinning) describes the length and thickness of the cervix relative to its normal state. It is usually reported as a percentage, from 0% (long, thick cervix) to 100% (completely effaced, paper-thin cervix). Points are given from 0 up to 3 for 80% or greater effacement.
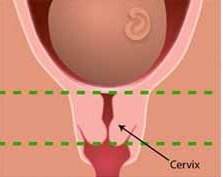
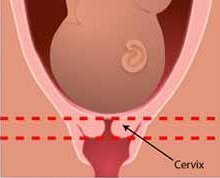
Image credit: National Institutes of Health, 2011.
Station
Station describes the position of the fetal head relative to the maternal ischial spines. Negative numbers (e.g., -3, -2) indicate that the head is above the spines; positive numbers (+1, +2) indicate that the head is below the spines. Station 0 is at the level of the spines. Points are given from 0 to 3 for stations progressing from -3 to +2.
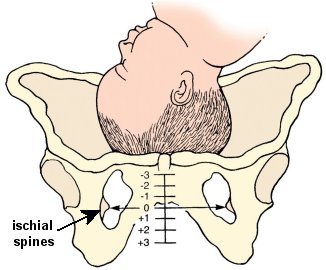
(c) LifeART / www.fotosearch.com Stock Photography
In 1988, the American College of Obstetricians and Gynecologists (ACOG) redefined station as the level of the leading bony point of the fetal head at or below the level of the maternal ischial spines, measured in centimeters (0–5 cm).
Consistency
Consistency describes how the cervix feels on digital examination:
- Firm: feels hard and rubbery.
- Medium: compressible but not soft.
- Soft: feels mushy, similar to the texture of the lips.
Position
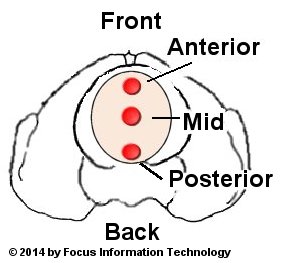
Position describes the orientation of the cervix in the pelvis. A cervix that is more anterior is generally associated with more advanced readiness for labor.
Reviewed by Mark Curran, M.D., FACOG
References
1. Bishop EH. Pelvic scoring for elective induction.
Obstet Gynecol. 1964;24:266–8.
PMID:
14199536
2. ACOG Practice Bulletin No. 107: Induction of labor. ACOG Committee on Practice Bulletins—Obstetrics.
Obstet Gynecol. 2009;114(2 Pt 1):386–97.
PMID:
19623003
3. Crane JM. Factors predicting labor induction success: a critical analysis.
Clin Obstet Gynecol. 2006;49(3):573–84.
PMID:
16885664
4. Spong CY, et al. Preventing the first cesarean delivery: summary of a joint NICHD/SMFM/ACOG workshop.
Obstet Gynecol. 2012;120(5):1181–93.
PMID:
23090537
5. Laughon SK, et al. Using a simplified Bishop score to predict vaginal delivery.
Obstet Gynecol. 2011;117(4):805–11.
PMID:
21383643.
Full text:
PMC3297470
6. Obstetric Forceps, ACOG Committee Opinion No. 59. Washington DC: American College of Obstetricians and Gynecologists; 1988.
7. Cunningham FG, Leveno KJ, Bloom SL, et al. Normal Labor and Delivery.
In: Williams Obstetrics, 23rd ed.; 2010:392.
8. Xenakis EM, et al. Induction of labor in the nineties: conquering the unfavorable cervix.
Obstet Gynecol. 1997;90(2):235–9.
PMID:
9241300
All calculations must be confirmed before use. These results do not substitute for clinical judgment.
