beta hCG Doubling Time / Half-Life Calculator
Review and JavaScript by Mark A. Curran, M.D., F.A.C.O.G. (reformatted for mobile display).
This tool calculates the approximate doubling time or half-life of serum beta human chorionic gonadotropin (β-hCG) between two measurements. It also reports the projected 2-day change assuming exponential kinetics and the observed percent change between the two samples.
To use the calculator:
- Enter the date and β-hCG value for the first blood sample.
- Enter the date and β-hCG value for the second blood sample.
Clinical Context
Ultrasonography is the preferred method to verify the presence of a viable intrauterine gestation.1 A gestational sac is usually seen at 5 weeks, a yolk sac at approximately 5½ weeks, and an embryo with cardiac activity at around 6 weeks using transvaginal ultrasound.
The Society of Radiologists in Ultrasound Multispecialty Panel advises that the following findings on transvaginal ultrasound are diagnostic of pregnancy failure:2
- Crown–rump length (CRL) ≥ 7 mm and no detectable heartbeat
- Mean sac diameter ≥ 25 mm and no embryo
- Absence of an embryo with heartbeat ≥ 2 weeks after a scan that showed a gestational sac without a yolk sac
- Absence of an embryo with heartbeat ≥ 11 days after a scan that showed a gestational sac with a yolk sac
The National Institute for Health and Care Excellence (NICE) recommends that if pregnancy failure is suspected, a second opinion and/or a repeat ultrasound be obtained at least 7 days after the first ultrasound examination before making a definitive diagnosis.3
A positive urine or serum pregnancy test with no intrauterine or ectopic pregnancy seen on transvaginal ultrasound is termed a pregnancy of unknown location. This may represent an early viable intrauterine pregnancy, a nonviable intrauterine pregnancy, or an ectopic pregnancy. The serum β-hCG value above which an intrauterine gestational sac would be expected to be seen on ultrasonography in a normal pregnancy is called the discriminatory hCG level.2
In the presence of an empty uterus, the likelihood of a viable pregnancy decreases as the hCG concentration increases. For example, at hCG levels of 2,000–3,000 mIU/mL, an estimated 2% of pregnancies will be viable, 65% nonviable, and 33% ectopic. At hCG levels > 3,000 mIU/mL, approximately 0.5% of pregnancies will be viable, 66.3% nonviable, and 33.2% ectopic.2 Nonetheless, live singleton births have been reported even when hCG levels exceeded 4,000 mIU/mL and no intrauterine gestational sac was seen on the initial ultrasound. The discriminatory level varies according to assay, ultrasound quality, and operator experience, and may be higher in multiple gestations. There is no absolute hCG level that is diagnostic of ectopic pregnancy.2,4,5
Serial serum β-hCG measurements every 48 hours may help determine the viability of early intrauterine pregnancies and guide management of pregnancies of unknown location in hemodynamically stable patients.5 One widely cited expectation is that the minimal rise over 48 hours is approximately 49% for an initial hCG < 1,500 mIU/mL, 40% for an initial level of 1,500–3,000 mIU/mL, and 33% for an initial level > 3,000 mIU/mL.6
Morse and colleagues (2012) suggested that for a successful intrauterine pregnancy, the β-hCG level should increase by at least 35% in 2 days. A slower rate of rise raises concern for miscarriage or ectopic pregnancy. In women having a miscarriage, β-hCG typically falls 36–47% over 2 days; a slower decline is worrisome for ectopic pregnancy. Approximately 21% of ectopic pregnancies demonstrate a rise in β-hCG similar to intrauterine pregnancies and 8% show a fall similar to that seen in miscarriage.7 Serial hCG values should always be interpreted in combination with clinical findings and repeat ultrasound when indicated.
Reference Ranges for β-hCG (First Half of Pregnancy)
Reference ranges below (using the Roche Cobas® analyzer) are typical examples; local laboratory reference values may differ.8
| Week of gestation | β-hCG (mIU/mL) | Chart |
|---|---|---|
| 3 | 6 – 71 |
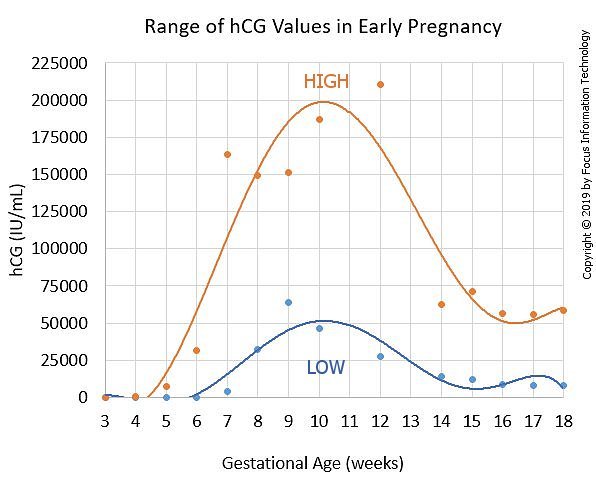 View chart in a new window
View chart in a new window
|
| 4 | 10 – 750 | |
| 5 | 217 – 7,138 | |
| 6 | 158 – 31,795 | |
| 7 | 3,697 – 163,563 | |
| 8 | 32,065 – 149,571 | |
| 9 | 63,803 – 151,410 | |
| 10 | 46,509 – 186,977 | |
| 12 | 27,832 – 210,612 | |
| 14 | 13,950 – 62,530 | |
| 15 | 12,039 – 70,971 | |
| 16 | 9,040 – 56,451 | |
| 17 | 8,175 – 55,868 | |
| 18 | 8,099 – 58,176 |
References
- Early pregnancy loss. ACOG Practice Bulletin No. 200. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2018;132:e197–207.
- Doubilet PM, Benson CB, Bourne T, Blaivas M, Barnhart KT, Benacerraf BR, et al. Diagnostic criteria for nonviable pregnancy early in the first trimester. N Engl J Med. 2013;369:1443–51.
- National Institute for Health and Care Excellence (NICE). Ectopic pregnancy and miscarriage: diagnosis and initial management. NICE Guideline NG126; 2019.
- Doubilet PM, Benson CB. Further evidence against the reliability of the human chorionic gonadotropin discriminatory level. J Ultrasound Med. 2011;30(12):1637–42. PMID: 22123998.
- Tubal ectopic pregnancy. ACOG Practice Bulletin No. 193. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2018;131:e91–103.
- Barnhart KT, et al. Differences in serum human chorionic gonadotropin rise in early pregnancy by race and value at presentation. Obstet Gynecol. 2016;128(3):504–11. PMID: 27500326.
- Morse CB, et al. Performance of human chorionic gonadotropin curves in women at risk for ectopic pregnancy: exceptions to the rules. Fertil Steril. 2012;97(1):101–6.e2. PMID: 22192138.
- Human Chorionic Gonadotropin (hCG) on Elecsys 1010/2010 and Modular Analytics E170 [package insert]. Indianapolis, IN: Roche; 2007–2009.
Disclaimer: All calculations must be confirmed before use. These results are not a substitute for clinical judgment. Neither Perinatology.com nor any other party involved in the preparation or publication of this site shall be liable for any special, consequential, or exemplary damages resulting in whole or in part from any user's reliance upon this material.
