Pap smear (Papanicolaou smear)
A screening method for cervical cancer named after George Papanicolaou (1883–1962), the American cytologist who developed this method. Using an Ayers spatula (and sometimes a brush or a plastic-fronded broom) cells are taken from the endocervical canal and transitional zone of the cervix and smeared thinly on a glass microscope slide. The slide is then sprayed or immersed in a fixative to be examined later for abnormalities in the laboratory.
Para, Parity
The number of completed pregnancies beyond 20 weeks gestation (whether viable or nonviable). The number of fetuses delivered does not determine the parity. For example, a woman who has been pregnant once and delivered twins at 38 weeks would be noted as Gravid 1 Para 1.
References
1. Cunningham FG, ed. Williams Obstetrics, 22nd ed. New York: McGraw-Hill; 2005.
2. Morgan M, Siddighi S. NMS Obstetrics and Gynecology. 2004; p.45.
Parenteral Nutrition (Total parenteral nutrition, partial parenteral nutrition, Hyperalimentation)
Substances necessary for life and growth such as carbohydrate, proteins, and fat fed directly into a vein. Usually given to people who are not able to take food by mouth.
Patent Ductus Arteriosus (PDA)
Failure of the blood vessel (called the ductus arteriosus) to close after birth. The ductus arteriosus is a normal structure in the fetus that diverts blood from the fetal lungs by connecting the pulmonary artery directly to the ascending aorta.
Pediatrician
A physician who has completed specialty training in the development, care, and diseases of children.
Pelvic inflammatory disease (PID, acute salpingitis)
A general term for inflammation caused by infection of the upper genital tract not associated with pregnancy or pelvic operations.
Percent transferrin saturation (TSAT)
Transferrin saturation (%) = {serum iron concentration (µg/dL) / TIBC (µg/dL)} × 100.
(Serum iron / TIBC) × 100%.
Percutaneous umbilical blood sampling (PUBS)
A procedure in which a needle is inserted into the uterus and into the umbilical cord of the fetus at the base of the placenta. A sample of fetal blood is then withdrawn.
Perinatal
Around the time of birth. As defined by the World Health Organization (WHO) ICD-10, the perinatal period begins at “22 completed weeks (154 days) of gestation (the time when birthweight is normally 500 grams) and ends seven completed days after birth.”
Perinatologist
A physician who has completed specialty training in obstetrics and gynecology and additional subspecialty training in high-risk pregnancy and disorders of the fetus. Also called a maternal–fetal medicine specialist.
Perinatal mortality rate (PNMR)
The number of perinatal deaths (fetal deaths at 22 weeks’ or more gestation and neonatal deaths to 7 completed days after birth) per 1,000 total births. It is usually reported on an annual basis.
Pfannenstiel’s incision (Bikini incision)
A horizontal cut made through the skin just above the joint of the pubic bones. The incision is carried down through the underlying fat and through the fibrous tissue that surrounds the rectus muscles of the abdomen (the anterior rectus fascia).
The incision was developed by the German gynecologist Hermann Johannes Pfannenstiel and provides an excellent cosmetic result. However, the incision does not provide good access to the upper abdomen.
Placenta (Afterbirth)
A disk-shaped organ that develops during pregnancy. The placenta is attached to the uterus on one side by its large flat surface and to the fetus by the umbilical cord on its other side. The placenta exchanges nutrients, wastes, and gases between the blood of the mother and fetus as well as producing numerous hormones. Normally the placenta is delivered after the birth of the infant.
Placenta Accreta, Increta, Percreta
Abnormal penetration of the placenta beyond the lining of the uterus to varying depths:
- Placenta accreta: The placenta adheres directly to the myometrium (muscular wall of the uterus).
- Placenta increta: The placenta grows into the myometrium.
- Placenta percreta: The placenta grows completely through the myometrium.
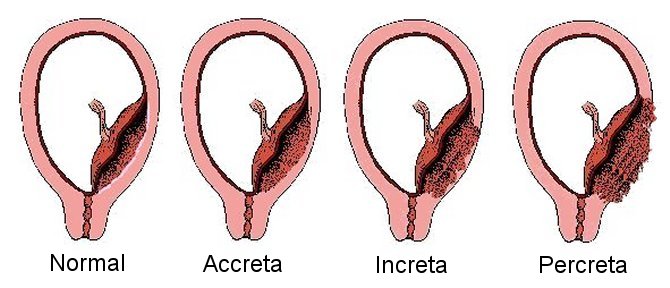
The abnormally firm attachment of the placenta to the uterus does not allow the placenta to separate from the uterine wall spontaneously after delivery of the fetus. Attempts to manually remove the placenta may sometimes cause massive bleeding. Placenta percreta may cause damage to nearby organs such as the bladder.
Placental insufficiency
Failure or inability of the placenta to normally exchange nutrients, wastes, and gases between the blood of the mother and fetus. The typical pathological finding in placental insufficiency is obliteration of the small muscular arteries in the tertiary stem villi of the placenta, which is often associated with an abnormal uterine artery waveform on pulsed-wave Doppler ultrasound.
See also: Umbilical Artery (UA) Impedance Indices.
References
1. Giles WB, et al. Fetal umbilical artery flow velocity waveforms and placental resistance:
pathological correlation. Br J Obstet Gynaecol. 1985;92(1):31–8. PMID: 3966988
2. Kingdom JC, Burrell SJ, Kaufmann P. Pathology and clinical implications of abnormal umbilical
artery Doppler waveforms. Ultrasound Obstet Gynecol. 1997;9(4):271–86. PMID: 9168580
3. Baschat AA, Weiner CP. Umbilical artery Doppler screening for detection of the small fetus in need
of antepartum surveillance. Am J Obstet Gynecol. 2000;182(1 Pt 1):154–8. PMID: 10649171
Placenta previa
The placental edge covers the internal cervical os (opening of the cervix).
Reference
Reddy UM, et al. Fetal imaging: Executive summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, American Institute of Ultrasound in Medicine, American College of Obstetricians and Gynecologists, American College of Radiology, Society for Pediatric Radiology, and Society of Radiologists in Ultrasound fetal imaging workshop. J Ultrasound Med. 2014;33(5):745–57. PMID: 24764329.
Placental lakes (placental vascular lacunae, placental caverns, placental venous lakes, placental sonolucencies)
Placental lakes are enlarged spaces in the placenta filled with maternal blood, also called intervillous vascular spaces. More...
Placental villi
Finger-like projections of the placenta that contain fetal blood vessels. The villi are surrounded by spaces containing maternal blood (the intervillous space).
Ponderal index (PI)
A ratio of body weight to length used as an indicator of asymmetric fetal growth status. The Ponderal index makes the assumption that the length is unaffected by changes in nutritional status.
Expressed as:
PI = [birth weight (g) × 100] ÷ [birth length (cm)]3
Normal range: 2.32 to 2.85 g/cm3
Reference
Gozal D, et al. Anthropometric measurements in a newborn population in West Africa: a reliable and simple tool for the identification of infants at risk for early postnatal morbidity. J Pediatr. 1991;118(5):800–5. PMID: 2019937.
Positive end expiratory pressure (PEEP)
The amount of pressure above atmospheric pressure in the airway at the end of the expiratory cycle. PEEP improves exchange of oxygen and carbon dioxide by preventing collapse of the small air sacs (alveoli) in the lungs.
Postpartum
Following birth.
Postpartum blues
A common (up to 70% of women) self-limiting condition occurring within a few days of delivery. Characterized by mood lability, weeping, depression, fatigue, anxiety, confusion, difficulty concentrating, and depersonalization.
A condition (~10%) occurring within days to weeks following delivery and lasting more than 2 weeks. Characterized by vegetative signs of depression, tearfulness, anxiety, loss of interest in normal activities, guilt, and inadequacy in coping with the infant, and may include thoughts of suicide. Risk factors for developing postpartum depression include previous depression and an unsupportive home environment. Typically requires treatment for up to 6 months with antidepressants. Psychiatric consultation may be helpful.
Postpartum psychosis
Uncommon condition occurring within a few days and up to 4 weeks after delivery. Characterized by auditory hallucinations, delusions, euphoria, grandiosity, hyperactivity, and inappropriate affect. There is a high risk of infanticide and a high chance of developing psychosis in the future. Risk factors for developing postpartum psychosis include a history of psychosis. Treatment usually requires hospitalization.
Pregnancy induced hypertension (PIH)
Old term for gestational hypertension. “The term PIH (pregnancy-induced hypertension) should be abandoned, as its meaning in clinical practice is unclear.”
References
1. Report of the National High Blood Pressure Education Program Working Group on High Blood Pressure in
Pregnancy. Am J Obstet Gynecol. 2000;183:S1–S22. PMID: 10920346
2. Diagnosis and management of preeclampsia and eclampsia. ACOG Practice Bulletin No. 33.
Obstet Gynecol. 2002;99:159–167. PMID: 16175681
3. Magee LA, Pels A, Helewa M, Rey E, von Dadelszen P; Canadian Hypertensive Disorders of Pregnancy
Working Group. Diagnosis, evaluation, and management of the hypertensive disorders of pregnancy:
executive summary. J Obstet Gynaecol Can. 2014;36(5):416–41. PMID: 24927294
Preeclampsia
A condition of pregnancy that affects the lining of the mother’s blood vessels causing high blood pressure, leaking of fluid from the blood vessels, and damage to multiple organs.
The American College of Obstetricians and Gynecologists (ACOG) recommends that preeclampsia should be diagnosed if the following conditions are met:
High blood pressure occurring for the first time after 20 weeks
- A systolic blood pressure (SBP) ≥ 140 mm Hg OR a diastolic blood pressure (DBP) ≥ 90 mm Hg on at least two occasions at least 4 hours apart
- A systolic blood pressure (SBP) ≥ 160 mm Hg OR a diastolic blood pressure (DBP) ≥ 110 mm Hg measured on more than one occasion several minutes apart
AND
- Protein in the urine (proteinuria): 300 mg or more in a 24-hour urine collection or a protein/creatinine ratio of at least 0.3 (each measured as mg/dL) . A result of 1+ on dipstick may be used only if the above methods are unavailable.
OR ANY OF THE FOLLOWING SEVERE FEATURES
- Cerebral or visual disturbances
- Pulmonary edema (fluid in the lungs)
- Low platelet count (less than 100,000 / microliter)
- Elevated liver enzymes (transaminases) to twice the normal concentration ( Normal Ranges for Transaminases in Pregnancy )
- Severe persistent pain in the right upper or middle upper abdomen that does not respond to medication and is not explained by another condition
- Renal insufficiency (serum creatinine > 1.1 mg/dL), or a doubling of serum creatinine in the absence of other renal disease
Women who develop high blood pressure for the first time after 20 weeks but do not have protein in their urine or severe features of preeclampsia are diagnosed with gestational hypertension (GHTN).
References
Hypertension in pregnancy: executive summary. Obstet Gynecol. 2013;122(5):1122–31.
doi:10.1097/01.AOG.0000437382.03963.88. PMID: 24150027
The American College of Obstetricians and Gynecologists. Task Force on Hypertension in Pregnancy.
Hypertension in Pregnancy. 2013.
Preterm
Less than 37 completed weeks’ (less than 259 days) of gestation.
